Summary
Clinical Notes can be added to the patient's record when adding treatment.
There are two methods of adding clinical notes:
The SOAP Method - History (subjective), Examination (objective), Diagnosis (assessment) & Plan.
Personalised Clinical Protocols - Implemented with an MWI Customer Product Consultant.
For information on Clinical Protocols, please contact your RCM or raise a ticket with support via the support portal or email support@mwiah.co.uk.
Add a Clinical Note
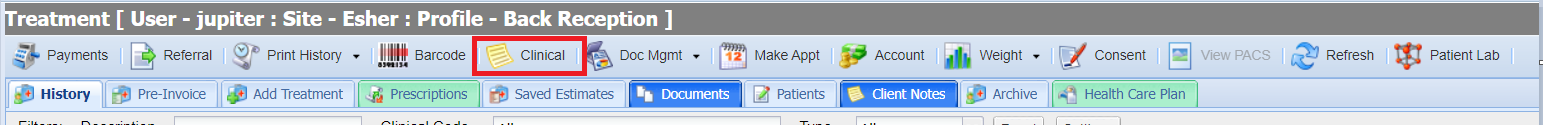
- Enter the Treatment Screen
- Select the 'Clinical' button
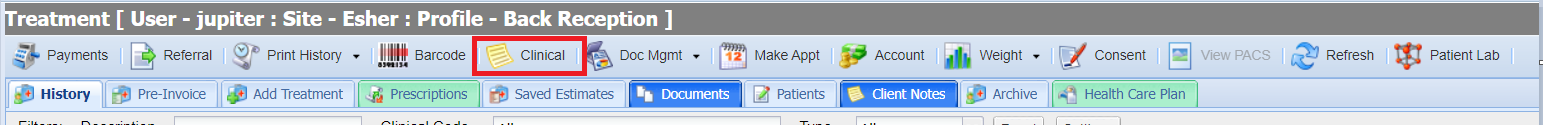 The Clinical notes window will display. The window displayed will depend on which clinical note method you have configured.
The Clinical notes window will display. The window displayed will depend on which clinical note method you have configured.
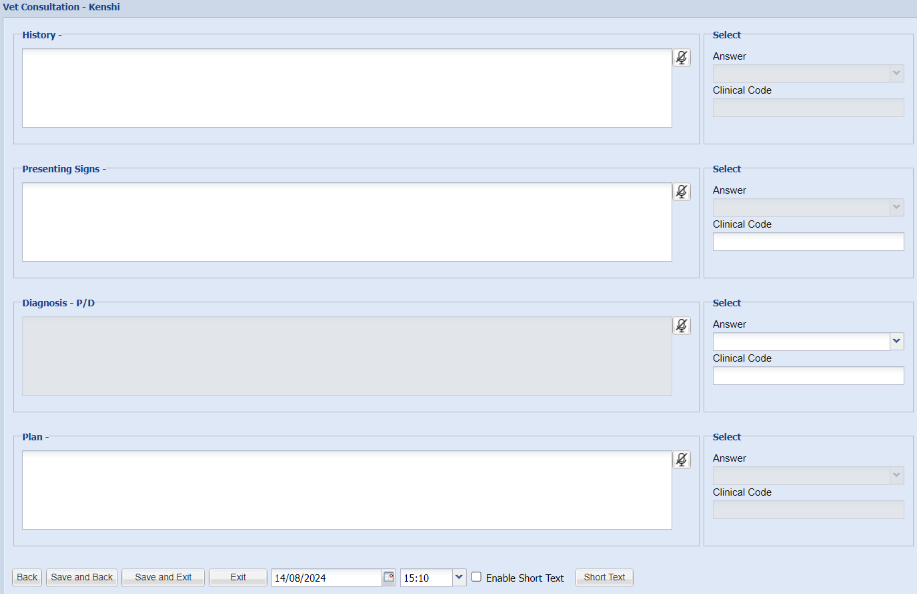
SOAP - Default Method
The default screen will display as below:
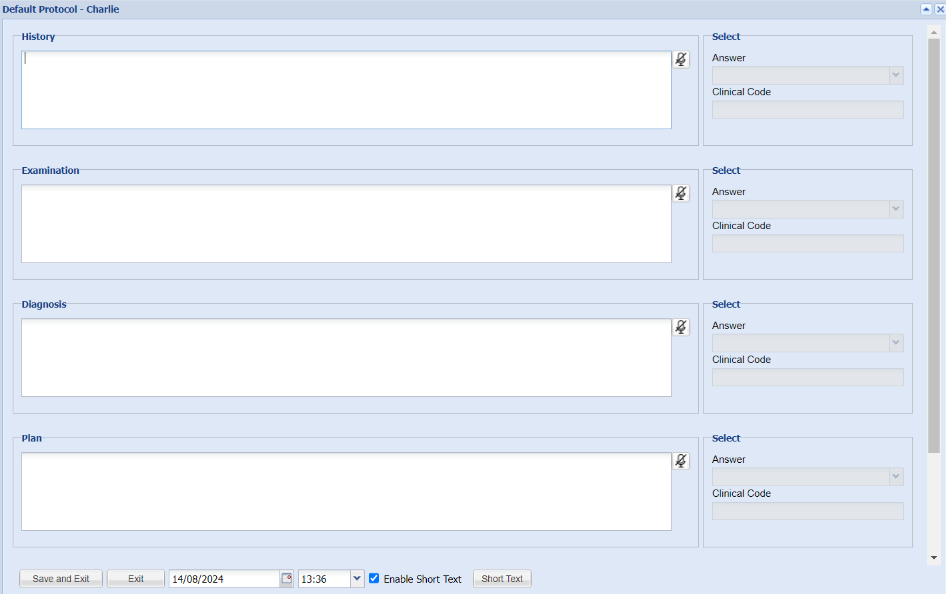
- The user can now type clinical notes in the boxes/answer fields provided.
- Once notes have been added, select 'Save and Exit' to add the notes to draft.
Note: Use the tab key on your keyboard or use the mouse to move from section to section.
Clinical Protocols - Alternative Method
If you want your practice/s to follow specific protocols, these can be configured with the assistance of an MWI Customer Product Consultant.
Think of these as consult specific headings, for example a weight clinic. You may want your clinical notes headings to be specific such as; Exercise Routine, Eating Habits, Mobility, Pain Score.
Selecting the 'Clinical' button will display a list of protocols.

- Select (double-click) the Protocol you wish to follow.
- The Clinical Notes screen will load.
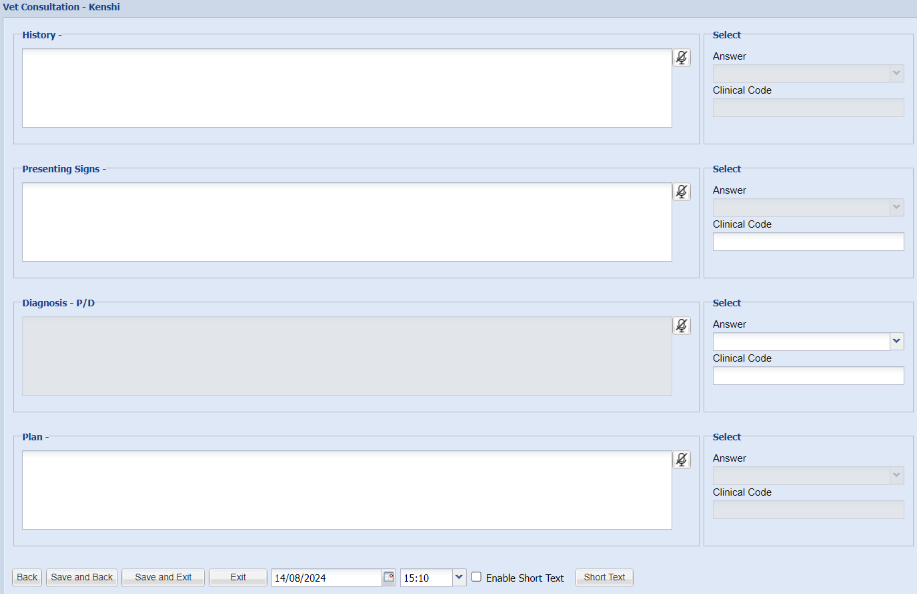
- The user can now type clinical notes in the boxes/answer fields provided. There is the ability to set some up as standard free text fields. Or some can have a set answer that displays in the drop down on the right hand side. You my also want a clinical code to be assigned for future reference.
- Once notes have been added, select 'Save and Exit' to add the notes to draft.
Note: Use the tab key on your keyboard or use the mouse to move from section to section.
Short Text
When in Clinical Notes you can enable Short Text. It is possible to enable or disable “Individual User Short Text Codes” for all users. For more on this see Treatment Settings

- Once Short Text is enabled, click on Short Text
- Enter the Name using a 4 letter limit
- Enter the Description. Paragraphing can be created by doing carriage returns (pressing enter) to create basic templates.

- When entering the Short Text type it and click on the space bar and the full description will display.

There is also the option to enable individual short text codes per user, instead of using the default shared library.
To turn this on, navigate to Administration > Settings > Treatment and enable individual short text codes. Once on each user will have a new blank library to build their own.
Saving Clinical Notes
Your notes will be saved into treatment draft. To save them to history, select the Save button.

Autosaving Clinical Notes to Drafts
If the setting for autosaving clinical notes is enabled, the clinical notes will be saved at intervals. After the predefined time (normally 5 minutes) the notes will be autosaved. An indicator at the bottom of the screen will show that the note has been autosaved.
The note will continue to be autosaved every 5 minutes. The session will remain open and the user logged in.
At any time the user can Save and Exit and the note will be appear as a draft in the Add Treatment Tab.
Before the note is autosaved, the user can press Exit. A warning will be displayed and, if they continue, the note will not be saved.
If a user does not interact with the clinical notes for an extended period (normally 4 hours) a warning message will be displayed asking them if they want to remain logged in. If they click Yes then the document will be autosaved again and the timer reset.
If they click No or do nothing, and no other interaction with the notes takes place, they will be logged out at the end of the normal session timeout. (i.e. If session timeout is 30 mins they will be logged out in approx 240 + 30 = 270 mins).
After being logged out, the user can log in and return to the autosaved notes. These are found in the Add Treatment tab for the patient. Autosaved notes have a different icon to normally saved notes. It is a disk with an exclamation mark. 
If the user tries to save autosaved draft notes to the patient history, a warning is displayed

If the user clicks Proceed, all the draft treatments in Add Treatment will be added to patient history, apart from any autosaved clinical notes, which will remain in draft.
The user can click on an autosaved draft note to edit it. After 5 minutes the note will be autosaved and the process continues as before. If the user exits the form using the window close icon [x] when creating a note, any autosaved draft note is deleted in the same way as happens when they use the Exit button. In edit mode using the close icon does not delete the autosaved note but displays a warning.
In any case, the autosaved note cannot be saved to the patient’s history until it is manually saved.
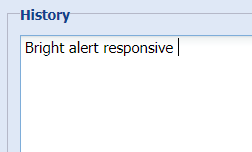
Speech-to-Text
If you are using a Google Browser, you can use your microphone to dictate clinical notes into the system.
When adding clinical notes, you will see a microphone button for each question.
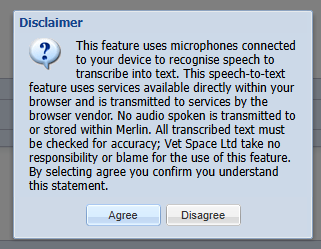
Using speech-to-text
- Select the microphone button.
- On first use, select ‘Agree’ to the disclaimer message.
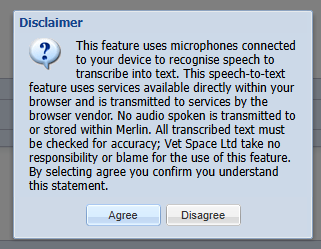
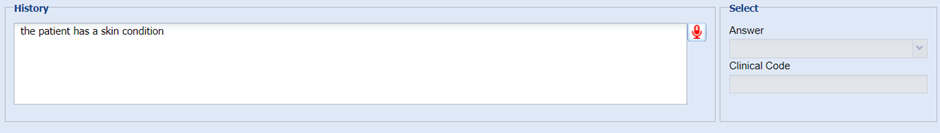
- The microphone button will appear red to indicate voice recording is in process.

- Once you have finished speaking, select the red microphone button to stop recording.
- Your speech will then be converted into text.
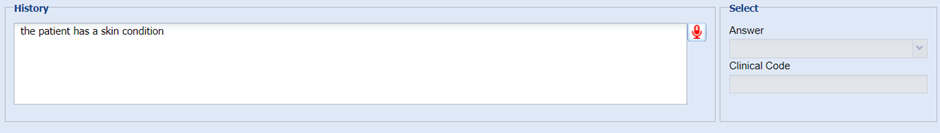
- Please check the text for accuracy before saving content into the Patient’s history.
 The Clinical notes window will display. The window displayed will depend on which clinical note method you have configured.
The Clinical notes window will display. The window displayed will depend on which clinical note method you have configured.